The literature supports the concept that combining multiple markers increases our ability to risk-stratify patients for cardiovascular risk. We have recently published the utility of combining inflammation tests to better define a patient’s risk.
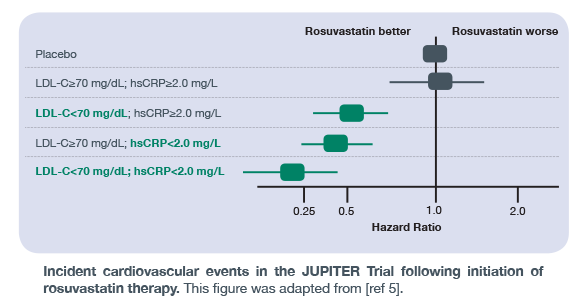
The JUPITER Trial was the first landmark trial to demonstrate increased identification and stratification of individuals at risk of adverse cardiovascular events using a multimarker approach. Prior to the results of this publication, most research focused solely on lowering LDL-C with statin therapy to reduce cardiovascular risk. The JUPITER Trial went beyond this traditional measurement to demonstrate that hsCRP, a marker of general- and cardiovascular-related inflammation within the body, can improve risk stratification of individuals who may benefit from rosuvastatin therapy. As shown in the figure here, individuals with low LDL-C, but high inflammation – as measured by hsCRP – had twice the risk of a cardiovascular event compared to individuals with low LDL-C and low hsCRP. These findings highlight the importance of a multimarker strategy in assessing cardiovascular risk, and measuring inflammation levels alongside traditional measurements such as LDL-C.
A Deeper Dive Into Inflammation
In addition to the landmark JUPITER Trial, other impactful, peer-reviewed publications exist that demonstrate the utility of a multimarker approach to individualize cardiovascular risk assessment. Multimarker approaches, when carefully designed with their physiological relevance in mind, can have additive utility of identifying the acuity of the risk.
Systemic and Vascular Inflammation
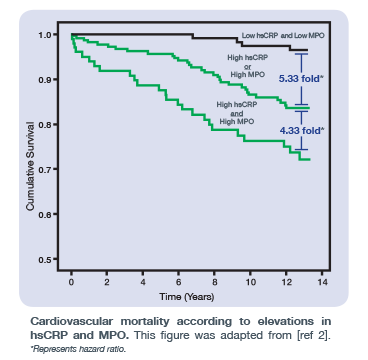
In 2009, Heslop et al. published a study in the Journal of the American College of Cardiology which examined the clinical utility of hsCRP and MPO – two inflammatory biomarkers with different pathophysiologies. Unlike hsCRP, free MPO within the bloodstream is a vascular-specific marker for vulnerable plaque formation. As shown in the figure here, individuals with elevated levels of both hsCRP (atheroma burden) and free MPO (active atheroma) in the bloodstream had approximately 4X increased risk of cardiovascular mortality compared to those with either hsCRP or MPO elevated.
Vascular Inflammation – Two Sides to the Story
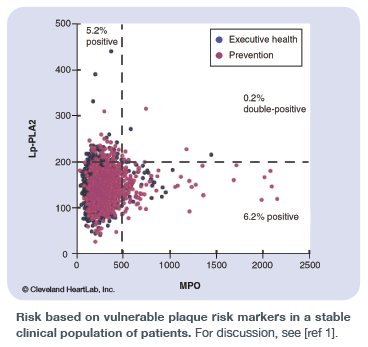
In 2013, Penn and Klemes published a study in Future Cardiology which examined the utility of a multimarker approach – when designed with the physiology of each marker in mind – to identify risk and ultimately acuity of risk. In particular, this study highlighted the ability of Lp-PLA2 and free MPO in the bloodstream to identify vulnerable plaque by measuring distinct physiologies. Lp-PLA2 examines macrophage activation underneath the collagen cap within the artery wall while free MPO examines the white blood cell response in the bloodstream due to vulnerable plaque/erosions/fissures in the artery wall. As shown in the figure here, the combined use of both Lp-PLA2 and MPO provides additional stratification of risk for plaque rupture beyond that of using each biomarker individually.
For more information and detailed references, please refer to our Clinical References page.

